Tiny ‘trampoline’ of human tissue will enable thousands to avoid shoulder replacement surgery
A tiny trampoline made of human tissue will enable thousands of patients to avoid shoulder replacement surgery, according to one of the world’s leading orthopaedic surgeons.
Patients with severely torn shoulder tendons are being treated with a new technique in which a membrane similar to the mat of a trampoline is used to reinforce the shoulder lining, Dr Stephen Burkhart told a recent meeting of the Arthroscopy Association of North America (AANA).
The new keyhole procedure will enable thousands of patients, who would once have had shoulder replacements, to preserve their natural shoulders.
“What is wonderful is that it has the potential to give a biological solution preserving the patient’s own natural shoulder as opposed to completely replacing it with a mechanical device prone to failure and higher rates of complications,” Dr Burkhart told our reporter. “That’s the appeal of it and so far the results are quite a bit better than the results of shoulder replacements so I think it holds a lot of promise.”
The technique is designed for massive irreparable rotator cuff tears. These are very common and among the most technically challenging injuries to treat in orthopaedic surgery.
The rotator cuff is made up of the muscles and tendons that keep the ball of the shoulder in the socket of the shoulder, enabling people to raise and rotate their arms.
Rotator cuff injuries usually happen in two ways: either a heavy fall suddenly rips the tendon or the tendon wears out gradually as the patient gets older. People who move their arms repetitively, such as painters or window cleaners, are particularly vulnerable as are older people. Patients experience pain, weakness and even paralysis in their arms.
Tears can range in severity from mild inflammation to complete holes in the tendon. Patients with mild tears are treated with physical therapy to strengthen the muscles in the shoulder joint whilst those with more serious tears may need surgical repair or transfer of alternative tendons.
However, it is people with massive irreparable rotator cuff tears (greater than 5cm), who will benefit from the new technique, which is called Superior Capsular Reconstruction (SCR). Previously these patients would have been candidates for total shoulder replacement.
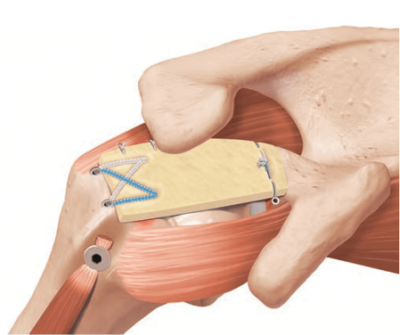
The technique involves shoring up the top of the shoulder lining (the superior capsule) with a graft of human tissue to prevent the ball of the shoulder from popping up or buttonholing through the torn tendons. It was first developed by Dr Teruhisa Mihata, a Japanese orthopaedic surgeon.
“Dr Mihata introduced the concept of covering the top of the rotator cuff with a graft,” said Dr Burkhart, who is based at The San Antonio Orthopaedic Group in San Antonio, Texas. “He attached the tissue with suture anchors at the top of the socket and then stretched it over to the ball part like a reverse trampoline.
“I wasn’t convinced it was going to work but he did a very elegant biomechanics study in a well respected lab in California. It was a compelling argument. The only other option for these people is shoulder replacement but if you can preserve their own natural biological shoulder then naturally that is the best.”
He added: “The problem with the reverse total shoulder replacement is that you have to sacrifice a lot of the bone in the shoulder to accommodate the mechanism of the replacement so if you then have to revise it later there is not a lot of bone to work with. For that reason, revisions haven’t always been satisfactory or even possible. After about seven or eight years the function of these reverse total shoulders rapidly goes down.
“I thought it would be worthwhile to try it Dr Mihata’s technique because it doesn’t burn any bridges – if it doesn’t work you can still do a shoulder replacement as a secondary procedure.”
Dr Burkhart performed his first superior capsule reconstruction three years ago and has since done 102 cases, he told an international gathering of orthopaedic surgeons organised by the AANA in Chicago, Illinois.
“The results have been great,” he said. “We ask patients: ‘What percentage of normal is your shoulder?’ On average at the end of the year, patients are saying their shoulders are 86% of normal. On average before the operation they said their shoulders were 24% of normal so we have made a jump from 24% of normal to 86%.
Out of 102 operations, there have been two failed procedures that have had to be revised.
Our principal Mr Simon Moyes, who attended the event in Chicago, said: “A lot of people, particularly in their fifties, sixties and seventies have chronically torn tendons in their shoulders that are irreparable. They are in chronic pain and often can’t move their arms.
“Their only option is total shoulder replacement. Although this is a good operation, it is a big surgery and the artificial joints wear out. This new technique is a much better solution, especially for older people who want to avoid major surgery. The results presented at the AANA in America were very impressive and over the past six to 12 months feedback from colleagues around the world has also been good. We have therefore just started offering the procedure at the Wellington Hospital.”
The operation
Superior Capsular Reconstruction (SCR) is not major surgery like a total shoulder replacement but it is a complex and challenging procedure.
Dr Burkhart makes a small incision and inserts the arthroscope into the shoulder. He identifies the rotator cuff tear and repairs whatever is repairable by attaching little suture anchors to the bone and then passing sutures from the anchors through the torn tendon and tying the ends together to bring the tendon down to the bone.
If there is a more serious tear it will typically be in the top of the shoulder. If it is not treated, the ball of the shoulder will buttonhole up through the gap in the torn tendon.
The SCR technique involves reinforcing the top lining of the shoulder (the superior capsule) with human tissue. Dr Burkhart uses donor tissue sourced from the skin of the lower back. This is the thickest skin in the human body (about 3mm) making it ideal for replicating the shoulder lining.
He attaches suture anchors to the bones on either side of the tendon defect and uses an arthroscopic measuring probe to measure the distance between the anchors. He then opens a packet of donated human skin and uses these measurements to shape it.
He shuttles the tissue through a cannula using sutures as a pulley system. He stretches the donor skin from the socket of the shoulder to the ball creating a tiny reverse trampoline, which prevents the ball from buttonholing through the gaps in the damaged tendon.
The arm is immobilised in a sling for six weeks and the patient is then given a stretching programme to get their motion back. Four months after the operation the graft should have healed enough for them to embark on a strengthening programme and they should be able to function fairly normally somewhere between eight and 12 months after the procedure.
